Background
Acute Myeloid Leukemia (AML) has a median age at diagnosis of 67 years. The only curative therapy remains an allogeneic hematopoietic stem cell transplant (HCT), yet it is complicated by non-relapse mortality (NRM) and ongoing morbidity including graft versus host disease (GVHD) that may impact survival, particularly in older patients. We examined the outcomes and predictors of success in a large cohort of patients aged 60 years and older receiving a HCT for AML in first complete remission (CR1).
Methods
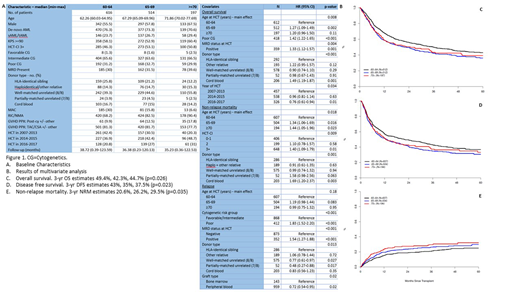
HCT recipients 60 years or older with AML in CR1 reported to the CIBMTR were included. Cox models were used to compare rates of overall survival (OS), disease-free survival (DFS), non-relapse mortality (NRM), relapse, acute GHVD, chronic GVHD in 3 separate age groups: 60-64 years vs. 65-70 years vs. 70+ years (Figure 1A).
Results
1,327 patients undergoing HCT from 2007-2017 were included. The three age cohorts (60-64; 65-69; 70+) were comparable in demographic and disease characteristics, except the older cohort had more males, more de novo AML, and a higher incidence of measurable residual disease (MRD) pre-HCT. Fewer had sibling donors and more were performed in recent years. With median follow-up of nearly 3 years, patients aged 60-64 had significantly better OS, DFS and lower NRM than those aged 65-69 and 70+. Those aged 65-69 and 70+ had similar outcomes (Figure 1). Three-year OS for the 3 cohorts was 49.4%, 42.3%, and 44.7% respectively (p=0.026). NRM was higher with increasing age, cord blood as graft source and HCT-CI score of ≥ 3. Conditioning intensity was not a significant predictor of outcomes with HR for OS for 60-69 cohort of 0.46 for RIC and 0.49 for MAC (p=0.38). There was no difference in the relapse rate, incidence of G3/4 acute GVHD, or incidence of moderate-severe chronic GVHD across the age cohorts. Poor risk cytogenetics, presence of MRD prior to HCT, cord blood as graft source, and transplant prior to 2016 were significant predictors of poor OS.
Discussion
In this large retrospective series of HCT for AML in CR1, age had a small effect OS and NRM after accounting for other predictors. High-risk features such as poor cytogenetics and presence of MRD prior to HCT were significantly associated with relapse and accounted for most of the adverse impact on OS and DFS. Age did not influence the incidence of either acute or chronic GVHD; graft type and associated GVHD prophylaxis were most important. These data suggest that age alone is not a barrier to successful HCT for AML in CR1 and should not exclude patients from HCT. Efforts should focus on minimizing residual disease and better donor selection.
Kebriaei:Ziopharm: Other: Research Support; Novartis: Other: Served on advisory board; Jazz: Consultancy; Amgen: Other: Research Support; Kite: Other: Served on advisory board; Pfizer: Other: Served on advisory board. Weisdorf:FATE Therapeutics: Consultancy; Incyte: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.